An “older people’s sounding board” is giving clinicians, consultants and service designers in the NHS direct access to the lived experiences of service users. Tony Watts OBE attended a recent meeting organised by the NDTi to find out what was being achieved.
A few weeks back, I was privileged to sit in on a day where representatives of the NHS England Older People’s Sounding Board met up with consultant surgeons and policy makers to give their feedback on projects designed to improve the way services are designed and delivered. I was there feeling at least a modicum of personal involvement, as the Age Action Alliance and EngAgeNet had played a role in recruiting this year’s new intake – a broad cross section of people from right across the country.
It was, in many ways, an enlightening experience. The quality of responses from the representatives was exceptional: asked for their input by senior clinicians, they were articulately and concisely relaying their opinions as well as their lived experiences – to not only provide a reality check on what would and wouldn’t work, but also providing incredibly helpful suggestions to improve outcomes.
The topics under discussion on this particular day centred on ways to deliver more NHS services within the home environment: specifically, enabling patients to return home more quickly after joint replacements or to keep those who had broken a bone in a “holding pattern” at home until the optimum time to bring them in for surgery.
Of course, this can’t work for everyone, but as one of the consultants explained to me, the potential benefits in terms of increasing the number of patients who can be treated with the same amount of resources (thus reducing waiting lists and costs) are huge. Enabling older people to get back into the comfort of their own home was another potential boon.
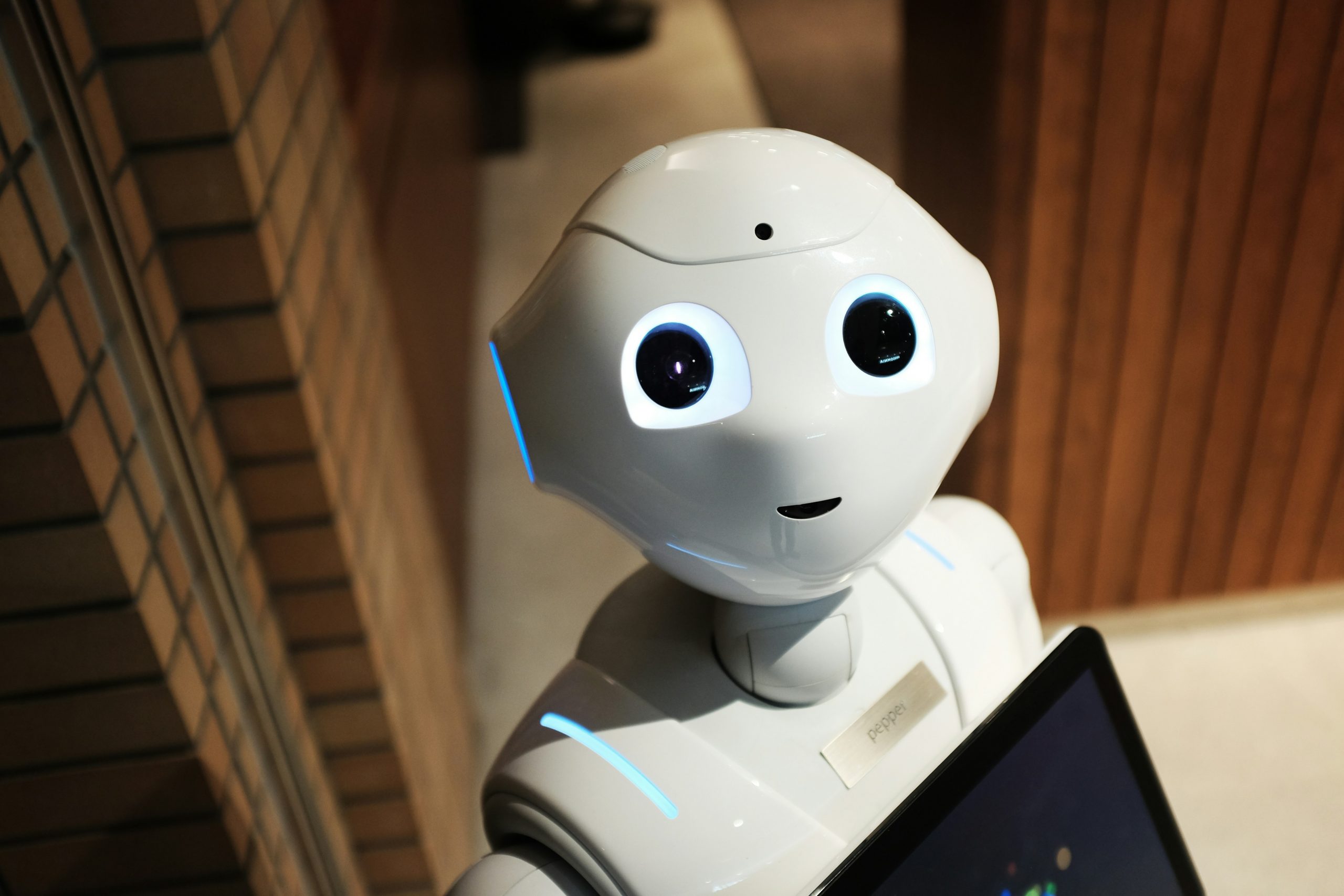
The way health services are designed and delivered is changing – fundamentally and rapidly. Root and branch change is inevitable, in order to cope with the changing demographics that are putting increasing levels of strain on already-overloaded systems. The potential of new technologies (notably AI, robotics and remote monitoring) to deliver “more bang per buck” has to be exploited to the full.
But in an increasingly data-driven environment, one basic fact can never be ignored: people have to be front and centre of what is provided and delivered… and people are not machines. That’s why opening up a channel of communications between service providers and service users is so critical.
The Government is already funding more ways to harness robotics and AI to deliver more healthcare in non-hospital settings. “Virtual wards” are set to play an increasing role in the way healthcare is delivered in this country. Increasingly, care providers will, need to depend upon remote monitoring to ensure people are safe and well in their homes, and their families will be looking for the same reassurance.
Critically, as we enter a “brave new world” of robots, AI and digital health, the voice of the patients on how all that will look and feel from the user’s perspective is being heard through channels like The Older People’s NHS Sounding Board.
Photo by Alex Knight on Unsplash